Hyphema cases are majorly seen in eye hospitals emergency departments, here are the details of Hyphema, and How to Treat Hyphema and the management of its Complications.
Table of Contents
What is Hyphema?
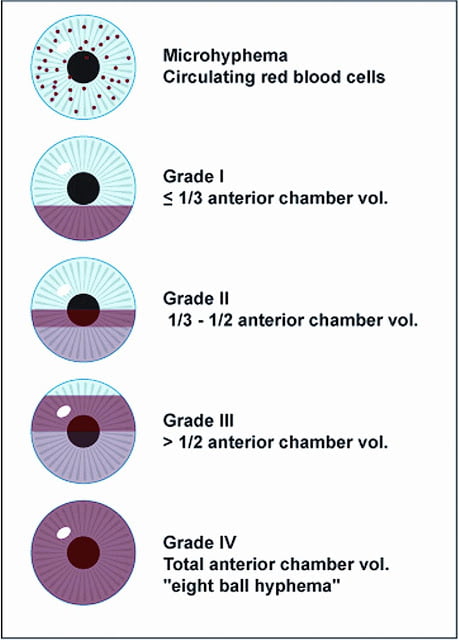
Hyphema is the medical term that defines the blood in the anterior chamber of the eye.

Hyphema Causes
- Blunt trauma is the most common cause of hyphema.
- Intraocular surgery
- Lacerating trauma,
- Penetrating & perforating injury
- It also occurs spontaneously without any trauma, usually neovascularization, a tumor of the eye (Retinoblastoma), uveitis or vascular anomalies.
- Using medicine that causes thinning of blood such as aspirin, ibuprofen etc.
Hyphema Symptoms
- Pain
- Photophobia
- Blurred vision
- Watering
Sign of Hyphema
- Blood or clot in the anterior chamber, usually visible without a slit lamp.
- Sometimes total hyphema (100%) may be present.
Pathophysiology of Hyphema
There are 2 suggested mechanism of hyphema formation
- The direct contusive force causes mechanical tearing of blood vasculature of iris and or angle.
- Concussive trauma creates rapidly rising intravascular pressure within the vessels resulting in rupture of vessels.
Blood in the anterior chamber is not by itself necessarily harmful. However, if quantities are sufficient it may obstruct the outflow of aqueous humour, resulting in glaucoma.
Examination and Workup
First of all, while managing the case of Hyphema, you have to carefully take the history of the patient. While taking history remember to add these questions to get an appropriate cause.
History
- Mechanism of injury? What object strikes the patients? How hard was the blow? Where did the blow strike?
- Uses of medications such as aspirin, ibuprofen, NSAIDs with anticoagulant properties. If yes ask for the duration since how long the patient is taking that medication.
- History of sickle cell disease.
Ocular Examinations
- Visual acuity examination
- Intraocular Pressure
- Slit-lamp examinations
- Hyphema height, location
- Cornea (to rule out perforation)
- The sclera (to rule out rupture globe)
- Anterior chamber and Pupillary reaction Lens, Vitreous, Retina
- B-scan ultrasonography (gently) if fundus view is poor due to the entire Anterior chamber filled with blood.
- If a suspected orbital fracture or Intra Ocular Foreign Body consider CT scan of orbit.
How to treat Hyphema and its complication
Main goals of Hyphema treatment
- To decrease the risk of re-bleeding within the eye.
- To decrease the risk of corneal blood staining.
- To decrease the risk of atrophy of the optic nerve.
- To prevent Peripheral anterior synechia.
Medical Treatment
- Hospitalization
- Strictly bed rest, Elevate the head to allow blood to settle.
- EyeShield at all the time.
- Dilating Drop Atropine 1% two times a day increases the comfort from traumatizing iris as well as reduce bleeding.
It prevents posterior and anterior synechia - Steroid Prednisolone acetate 1% (1 hourly- QID)
- It helps to reduce inflammations.
- If any suggestion of iritis, lens capsule rupture any fibrin is seen in the anterior chamber it is indicated. Tapper Steroid when sign and symptoms resolve to reduce steroid-induced glaucoma.
If Intra Ocular Pressure is increased
- Increased IOP especially seen after trauma, may be transient, secondary to acute mechanical plugging of the Trabecular Meshwork.
- Start with beta-blockers (Timolol 0.5%, Betaxolol).
IF IOP is still high- - Add topical alpha agonist (brimonidine 0.15%), TDS, it is contraindicated in children.
- Add Carbonic anhydrase inhibitor Gtt. Dorzolamide2% 1drop*TDS
- If topical therapy did not control IOP then start Tab Acetazolamide ( DIAMOX) 500mg* BD
Or Start IV MANITOL 1-2mg/kg
Indications for surgical evaluation of hyphema.
- Corneal stromal blood staining
- Significant visual detortion
- Hyphema that doesn’t decrease to more than or equals to 50% by 8 days (to prevent PAS)
- IOP equals to or more than 60mmofhg for 48 hours or more, despite maximal medical therapy (to prevent optic atrophy)
- IOP ≥ 25mmof hg with total hyphema for ≥ 5days (to prevent corneal stromal blood staining)
- IOP 24 mm of Hg for ≥ 24hours(or any transient increase in IOP ≥ 30 mm of Hg) in sickle disease patient.
- Consider early surgical intervention for children at risk of amblyopia.
Note
Gonioscopy is contraindicated because it increases the risk of rebleeding, perform it after the event has resolved and the risk of rebleeding is passed.
Complications
- Increased IOP
- Peripheral anterior synechiae
- Optic atrophy
- Corneal stromal blood staining
- Rebleeding
- Impaired accommodation.
How to Prevent Hyphema at Home
Hyphema can occur with any trauma to the eye, wear protective eyewear when playing and doing outwork.
Disclaimer: Please Consult with an Ophthalmologist for treatment. We do not suggest self-medication with reference to our site.
References:-
Wills eye manual, 6th edition
A.K Khurana’s comprehensive ophthalmology
www.ophthobook.com